 |
This peer-reviewed column does not represent official ASHRAE guidance. For more information on ASHRAE resources on COVID-19, visit ashrae.org/COVID19. |
Guidance for Building Operations During the COVID-19 Pandemic
By Lawrence J. Schoen, P.E., Fellow/Life Member ASHRAE
From ASHRAE Journal Newsletter, March 24, 2020
The HVAC systems in most non-medical buildings play only a small role in infectious disease transmission, including COVID-19.1 Knowledge is emerging about COVID-19, the virus that causes it (SARS-CoV-2), and how the disease spreads. Reasonable, but not certain, inferences about spread can be drawn from the SARS outbreak in 2003 (a virus genetically similar to SARS-CoV-2) and, to a lesser extent, from transmission of other viruses. Preliminary research has been recently released, due to the urgent need for information, but it is likely to take years to reach scientific consensus.
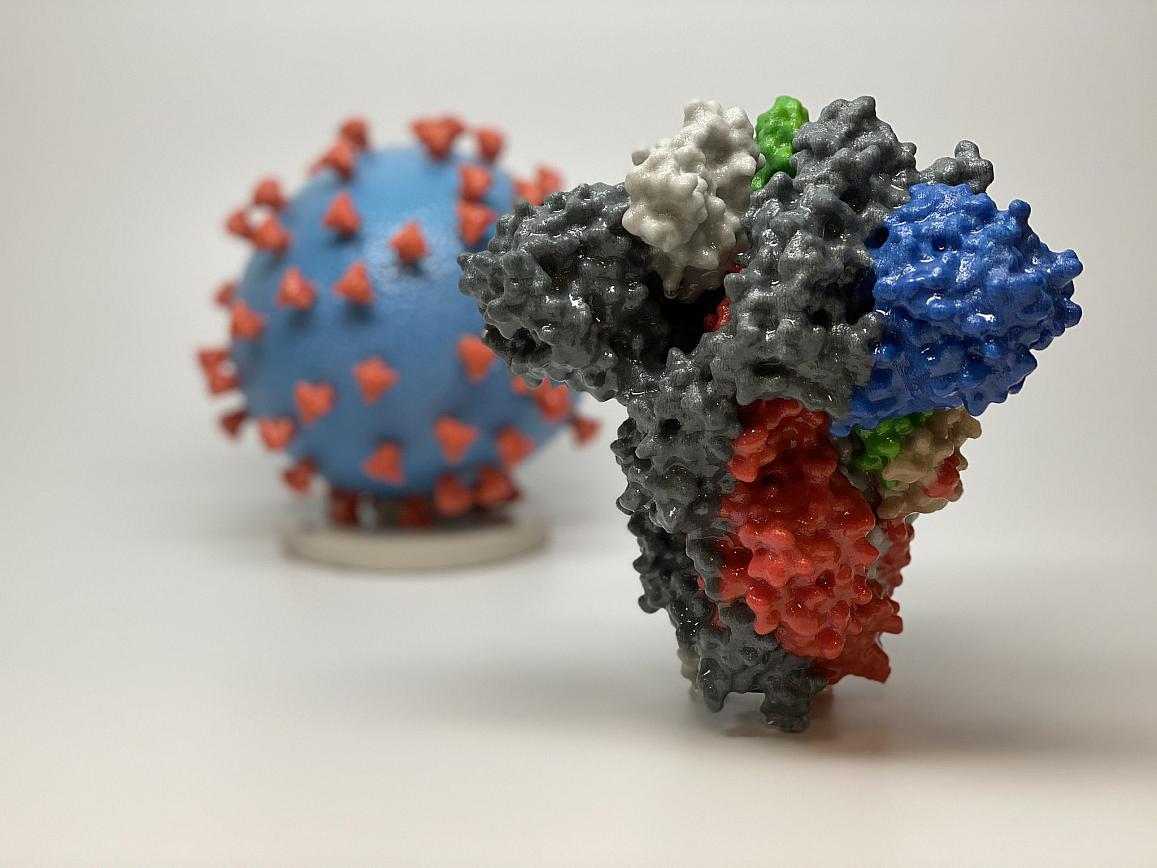
A 3D print of a spike protein of SARS-CoV-2—the virus that causes COVID-19—is shown in front of a 3D print of a SARS-CoV-2 virus particle. Credit: NIH
Even in the face of incomplete knowledge, it is critically important for all of us, especially those of us in positions of authority and influence, to exercise our collective responsibility to communicate and reinforce how personal choices about social distancing and hygiene affect the spread of this disease and its impact not just on ourselves, but on our societal systems and economy. The consequences of overwhelming the capacity of our health-care systems are enormous and potentially tragic. The sooner we “flatten the curve,”2 the sooner we can return to safer and normal economic and personal lives.
According to the WHO (World Health Organization), “The COVID-19 virus spreads primarily through droplets of saliva or discharge from the nose when an infected person coughs or sneezes….” Talking and breathing can also release droplets and particles.3 Droplets generally fall to the ground or other surfaces in about 1 m (3 ft), while particles (aka aerosols), behave more like a gas and can travel through the air for longer distances, where they can transmit to people and also settle on surfaces. The virus can be picked up by hands that touch contaminated surfaces (called fomite transmission) or be re-entrained into the air when disturbed on surfaces.
SARS infected people over long distances in 2003,4 SARS-CoV-2 has been detected as an aerosol in hospitals,5 and there is evidence that at least some strains of it remain suspended and infectious for 3 hours,6 suggesting the possibility of aerosol transmission. However, other mechanisms of virus dissemination are likely to be more significant, namely,
- direct person to person contact
- indirect contact through inanimate objects like doorknobs
- through the hands to mucous membranes such as those in the nose, mouth and eyes
- droplets and possibly particles spread between people in close proximity
For this reason, basic principles of social distancing (1 to 2 m or 3 to 6.5 ft), surface cleaning and disinfection, handwashing and other strategies of good hygiene are far more important than anything related to the HVAC system.7 In the middle-Atlantic region of the United States where I work, malls, museums, theaters, gyms and other places where groups of people gather are closed and there are “stay at home”8 orders. This is a “game” of chance, and the fewer individuals who come in close contact with each other, the lower the probability for spread of the disease. Since symptoms do not become apparent for days or weeks, each of us must behave as though we are infected.
Other public buildings, considered essential to varying degrees, remain open. These include food, hardware and drug stores, and of course, hospital and health-care facilities (which are beyond the scope of this article). Anecdotally, some universities are allowing some or all faculty, staff and graduate students to conduct essential research and online classes. Banks and other service organizations are open to staff and are receiving customers by appointment only, and private and government workplaces are open with work at home for some or all encouraged or mandated.
For those buildings that remain open, in addition to the policies described above, non-HVAC actions include:
- Increase disinfection of frequently touched surfaces.9
- Install more hand sanitation dispensers, assuming they can be procured.
- Supervise or shut down food preparation and warming areas, including the office pantry and coffee station.
- Close or post warning signs at water fountains in favor of bottle filling stations and sinks, or even better, encourage employees to bring their water from home.
Once the basics above are covered, a few actions related to HVAC systems are suggested, in case some spread of the virus can be affected:
- Increase outdoor air ventilation (use caution in highly polluted areas); with a lower population in the building, this increases the effective dilution ventilation per person.
- Disable demand-controlled ventilation (DCV).
- Further open minimum outdoor air dampers, as high as 100%, thus eliminating recirculation (in the mild weather season, this need not affect thermal comfort or humidity, but clearly becomes more difficult in extreme weather).
- Improve central10 air filtration to the MERV-1311 or the highest compatible with the filter rack, and seal edges of the filter12 to limit bypass.
- Keep systems running longer hours, if possible 24/7, to enhance the two actions above.
- Consider portable room air cleaners with HEPA filters.
- Consider UVGI (ultraviolet germicidal irradiation), protecting occupants from radiation,13 particularly in high-risk spaces such as waiting rooms, prisons and shelters.
Construction sites present unique challenges. Much, but not all, construction work has the recommended social distancing; much, but not all, is outdoors or in partially enclosed and therefore well-ventilated buildings; and many, but not all, workers already use personal protective equipment such as masks14 and gloves. Governments in some locations have mandated closure of construction sites, while in others work proceeds.15 Engineers who perform field observations, commissioning or special inspections must consider what work can be postponed, performed remotely, or conducted using photographic documentation, and what personal precautions to take when site visitation is unavoidable.
If you, the reader, are called upon to advise building operators, please use the above general guidance, and be sure to combine it with knowledge of the specific HVAC system type in a building and the purpose and use of the facility. Like all hazards, risk can be reduced but not eliminated, so be sure to communicate the limitations of the HVAC system and our current state of knowledge about the virus and its spread.
We all have a role to play to control the spread of this disease. HVAC is part of it and even more significant are social distancing, hygiene and the influence we can have on personal behavior.
Thanks to William P. Bahnfleth, Ph.D., P.E., Presidential Member/Fellow ASHRAE, Lew Harriman, Fellow ASHRAE, Yuguo Li, Ph.D., Fellow ASHRAE, Andrew K. Persily, Ph.D., Fellow ASHRAE, and Pawel Wargocki, Ph.D., Member ASHRAE for their review of preliminary drafts of this article. Any errors that remain are the author’s alone.
Lawrence J. Schoen, P.E., is president and principal engineer at Schoen Engineering, Inc. in Columbia, Md. He was chair of the committee that wrote the 2014 and 2017 versions of the “ASHRAE Position Document on Airborne Infectious Diseases.” The position document had been undergoing revision when this article was written and on April 14 was replaced with "Position Document on Infectious Aerosols."
Author’s note: ASHRAE published official guidance on 4/20/2020 on managing the spread of SARS-CoV-2 with respect to the operation and maintenance of heating, ventilating and air-conditioning systems in buildings, which can be found at https://www.ashrae.org/about/news/2020/ashrae-issues-statements-on-relationship-between-covid-19-and-hvac-in-buildings, and where the reader can also find links to additional resources. - L. Schoen 5/1/2020.
Endnotes
- According to the WHO, COVID-19 is the name given on February 11, 2020 by the ICTV (International Committee on Taxonomy of Viruses) to the disease caused by SARS-CoV-2, aka the novel coronavirus. Hospitals and health-care facilities are beyond the scope of this article, though many of the same principles apply to them.
- “NIH Director: ‘We’re on an Exponential Curve’”, The Atlantic, Peter Wehner, March 17, 2020.
- Bischoff 2013. References cited with only a name and date in this article are taken from ASHRAE Position Document on Airborne Infectious Diseases, 2014, 2020 (“PD”). According to the PD, there is no exact size demarcation between droplets and particles, and this “… is less important than knowing that large droplets and small particles behave differently and that the latter can remain airborne.”
- Yu et al. 2004; Li et al. 2005a, 2005b. References from ASHRAE Position Document on Airborne Infectious Diseases.
- “Aerodynamic Characteristics and RNA Concentration of SARS-CoV-2 Aerosol in Wuhan Hospitals during COVID-19 Outbreak,” non-peer reviewed preprint. bioRxiv, posted March 10, 2020.
- “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1,” letter to the editor New England Journal of Medicine, March 17, 2020, DOI: 10.1056/NEJMc2004973.
- Non-health care workplaces fall into the medium and lower exposure risk categories described in Guidance on Preparing Workplaces for COVID-19, U.S. Department of Labor, Occupational Safety and Health Administration OSHA 3990-03 2020.
- Stay at home orders have been incorrectly called “shelter in place.” The latter is a more extreme action advised when there is an outdoor contaminant, which is not the COVID-19 situation. See https://emergency.cdc.gov/planning/shelteringfacts.asp
- To paraphrase the words of the singer-songwriter Joe Jencks, janitors, cleaners, nurses, aides, doctors, EMTs and other first responders are our “viral firefighters,” the advance guard in the fight against this virus.
- This applies to systems that deliver air to the occupied space and, to a lesser extent, room air returned to rotary heat exchangers, in order to reduce cross contamination.
- MERV-13 Is approximately equivalent to F7, a rating used in the EU. More effective filters with reasonable pressure drop are available, and some increased pressure drop often results in an acceptably small effect on system performance.
- Consider the filters contaminated, protect personnel changing them, and seal them in plastic bags for disposal.
- There is research that shows UVGI in both the upper-room and in-duct configurations can inactivate some disease-transmitting organisms. Either of these takes time to plan and install. For more information, see the ASHRAE PD previously cited and Chapter 62 Ultraviolet Air and Surface Treatment of 2019 ASHRAE Handbook—HVAC Applications.
- N95 masks are in short supply and some contractors are donating them to medical facilities, according to Engineering News Record March 18, 2020 “Construction Firms Respond to Mask Donation Need.”
- Engineering News Record, March 19, 2020, “Pennsylvania Halts All ‘Non-Life-Sustaining Business” Operations, Including Construction.”
The Author Answers Reader Questions
From John H.
For buildings that are unoccupied and closed, is there any guidance on limiting the hours of operation of the HVAC systems related to the COVID-19 virus? This is a time when many buildings are not occupied. It might appear as an opportunity to save significant HVAC-related energy by either turning off HVAC systems or setting back the temperatures to a deep setback.
I have one client who insists that he must ventilate his completely unoccupied building at least eight hours per day. He does not site any evidence that this is needed and I have not seen any research or practice that suggests that a closed building needs to be ventilated. (Humidity control is always a consideration in buildings which might be a reason to maintain temperature, and possibly, ventilation rates depending on climate conditions).
Schoen: I’m not aware of a requirement to provide outside air to an unoccupied building, nor am I aware of any benefit or plausibility of benefit. When eliminating outside air, also turn off non-essential general and toilet exhaust systems. For exhaust systems that must remain operational, e.g., those serving battery rooms and electric rooms, provide makeup to avoid problems from pressure imbalance such as uncontrolled air flow through the building envelope.
The issue of ventilating for cleaning personnel who may be in the building is another issue, and I personally recommend it while they are cleaning, for dilution of the cleaning chemicals and in these times, to reduce their possible exposure to each other’s respiratory aerosols. Another maintenance task advisable is to keep plumbing traps full. Dry traps were found to be a factor in the 2003 SARS outbreak.
With regard to temperature and humidity, ASHRAE Standard 62.1-2019 has a requirement for “…maximum dew point of 60°F (15°C) during both occupied and unoccupied hours whenever the outdoor air dew point is above 60°F (15°C).” I’m not aware of upper or lower limits for temperature, except of course, to prevent freezing and perhaps the effect of too high a temperature on building materials such as wood flooring.
In preparation for occupancy, there is a protocol in Standard 189.1-2017 for a 14-day flush out prior to occupancy of newly constructed space, for the purpose of removing contaminants from construction and new furnishings. 189.1 also requires one hour of ventilation prior to occupancy when a space is unventilated for more than 24 hours. If unventilated for weeks, there is no specific practice guideline of which I am aware, but commencing ventilation the evening before morning occupancy seems to me to be a reasonable action.
From Taylor G.
You should note that these recommendations will increase operating costs at a time when building operators are likely seeking to reduce costs to adjust for lower revenues from business closings. Increasing energy costs by delivering 100% outdoor air on a 24/7 basis and incurring new equipment costs by installing UV-C lights, enhanced filtration and portable room air cleaners may not be feasible.
Schoen: Yes, following my recommendations will certainly increase cost, as do many of the actions we take during this pandemic. There are many people unemployed, underemployed and government programs to support the economy. While I’m not an economist, there seem to me ways to satisfy both the demand for control of infection and use under-utilized labor, capital, energy, and other resources.
From Joe C.
Is there any guidance with regards to the technician’s safety when changing filters in air handling units?
Schoen: You might consult hospital practice criteria and OSHA for worker protection. I have not consulted these resources, but it seems logical to me to use gloves, an N95 respirator (though these are admittedly in short supply) and put the filters in sealed plastic bags for disposal.
From Jim S.
What should be the recommendation for the K-12 schools that have closed as it pertains to ventilation during the closed period? I have noticed that the school districts have put their buildings to “Unoccupied.” Is it ok to keep the ventilation systems off? What would be the recommendation for these schools when it is time to re-open?
Schoen: See answer to John H. above.
From Mike M.
Will displacement ventilation systems help?
Schoen: I am aware of some studies in hospitals that show reduced exposure from the use of displacement ventilation. I’m not aware of similar study of the non-healthcare indoor environments that were the subject of my article. However, it seems logical that a typical displacement ventilation system would be more effective than ceiling supply at moving the personal contaminant cloud up to return grilles in the ceiling. Reduction in personal exposure to others would then seem plausible if this return air went to a central system that replaced some or all of it with uncontaminated outdoor air, combined with high MERV filtration.