Modes of Transmission | Airborne Transmission and Core Recommendations | Aerosol Generating Procedures | Secondary Infection | Cohorting – Cautions and current methods | Alternate Care Sites | Suggested Approaches | Guidance on Recirculation and Increased Outside Air Fraction | Consider Maintaining relative humidity at 40-60% RH | Suggested Approaches to Deactivate or Bypass Heat Recovery Wheels | Suggested Approaches to Improve/Consider Room Airflow Patterns | Utilize portable ante rooms with HEPA filtration | HEPA Filters | Facilities/Maintenance – PPE | HVAC System Maintenance and Filter Replacement | Filter Changing in units serving COVID-19 patients | Facilities/Maintenance | Disinfection | Emergency Department | Layered Approach – A Variety of Options | Source Control Options | Operating on a COVID-19 patient | Variable Air Volume Systems | Room Recirculating Units | Caution – Room Recirculating Units | 2--Person Patient Rooms | Cautions when using OR as Temp. ICU | Temporary Vestibule at OR | Warning on Older ICU Units | Gastrointestinal Endoscopy | Transmission through Air in Toilet Rooms | Gas/Vac Systems | Healthcare Team Members | Acknowledgements | Disclaimer
SARS-CoV-2, the virus that causes COVID-19, is transmitted by various pathways. One such pathway is person-to-person transmission through the inhalation of respiratory droplets when someone with COVID-19 coughs, sneezes, or talks. It has also been recognized that SARS-CoV-2 is transmitted through inhalation of smaller virus-containing aerosols over distances exceeding 12 feet in special settings. Current data do not support long range aerosol transmission as a primary transmission pathway, such as seen with measles or tuberculosis. To date, no data has documented the transmission of SARS-CoV-2 through HVAC systems and subsequently causing a COVID-19 infection, but that potential continues to be researched. has not been established.
See ASHRAE Statements on Airborne Transmission, and the Environmental Health Emerging Issue Brief, “Pandemic COVID-19 and Airborne Transmission”.
- Recognize That Virus May Be Aerosolized During Toilet Flushing even in subsequent flushes following inital use by an infectious person.
- Keeping plumbing traps full of water or mineral oil to avoid transmission of sewer aerosols through dry traps. SARS-CoV-1 and SARS-CoV-2 have both been shown to be transmitted this way, and two SARS-CoV-2 published studies posited transmission in a similar manner.
Airborne Transmission Statement & Core Recommendations | Return to Top
ASHRAE Statement on airborne transmission of SARS-CoV-2
- Airborne transmission of SARS-CoV-2 is significant and should be controlled. Changes to building operations, including the operation of HVAC systems can reduce airborne exposures.
ASHRAE Statement on operation of heating, ventilating, and air-conditioning systems to reduce SARS-CoV-2 transmission
- Ventilation and filtration provided by heating, ventilating, and air-conditioning systems can reduce the airborne concentration of SARS-CoV-2 and thus the risk of transmission through the air. Unconditioned spaces can cause thermal stress to people that may be directly life threatening and that may also lower resistance to infection. In general, disabling of heating, ventilating, and air-conditioning systems is not a recommended measure to reduce the transmission of the virus.
ASHRAE Core Recommendations for Reducing Airborne Infectious Aerosol Exposure are available HERE
Aerosol Generating Procedures | Return to Top
It is possible that the virus is spread through aerosol so it is preferred to minimize aerosol generating procedures.
- positive pressure ventilation (BiPAP and CPAP)
- endotracheal intubation
- airway suction
- high frequency oscillatory ventilation
- tracheostomy
- chest physiotherapy
- nebulizer treatment
- sputum induction
- Bronchoscopy
Secondary Infection Susceptibility | Return to Top
Secondary infections are a significant complicating factor for patients with COVID-19. There are studies that show a significant portion of patients with COVID-19 also acquire another infectious disease.
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study:
This study showed how developing a co-infection (secondary infection) from a hospital when a patient is dealing with COVID-19 increases the likelihood of death by 27 times.
- Precautions are Needed for COVID-19 Patients with Coinfection of Common Respiratory Pathogens:
Among COVID-19 patients in Qingdao, 80.00% of them had IgM antibodies against at least one respiratory pathogen, whereas only 2.60% of the patients in Wuhan had positive results for serum IgM antibody detection. The most common respiratory pathogens detected in Qingdao COVID-19 patients were influenza virus A (60.00%) and influenza virus B (53.30%), followed by mycoplasma pneumoniae (23.30%) and legionella pneumophila (20.00%). Legionella Pneumophila is a waterborne pathogen from the plumbing system and needs to still be addressed.
- Co-infection with SARS-CoV-2 and Influenza A Virus in Patient with Pneumonia, China:
We report co-infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and influenza A virus in a patient with pneumonia in China. The case highlights possible co-detection of known respiratory viruses. Low sensitivity of upper respiratory specimens for SARS-CoV-2 could further complicate recognition of the full extent of disease.
Cohorting – Cautions and current methods | Return to Top
- Clinicians have advocated against cohorting suspected and confirmed patients to avoid the potential for conversion. Coordinate with your clinical staff in this manner.
- Do designate specific area outside or in ED for respiratory cases
- In order to manage patient influx, congestion, and to control the risk of exposure to healthcare workers, consider designating a specific area in the ED for respiratory cases.
- Do triage Persons Under Investigation (PUI) capable of self-care outside the ED, either through drive-through or walk-up screening stations set up in tents or temporary spaces, and advised to continue home care until results are available.
- Do consider designating entire units to care for COVID patients
- Conserves PPE
- Improves containment
Clinical Goals Will Dictate Infrastructure Needed
- Determine if space is for COVID-19 Confirmed, suspected, or non-COVID-19 Patients and at what acuity level. Do not cohort suspected & confirmed patients. Consider locations for staff respite areas.
- Consider Liability Issues If Diverging From FGI/State Guidelines
- ASHE Note: During emergencies, it is important that activities be coordinated through the organization’s incident command system. Activities outside of an organization’s command structure should be coordinated with the local, county and state incident command systems. This enables effective and efficient incident management within common organizational structures.
CDC/NIOSH Info on "Expedient Patient Isolation Rooms"
ASHRAE and the US Army Corps of Engineers partnered to produce the Alternate Care Site HVAC Guidebook, available for free download HERE.

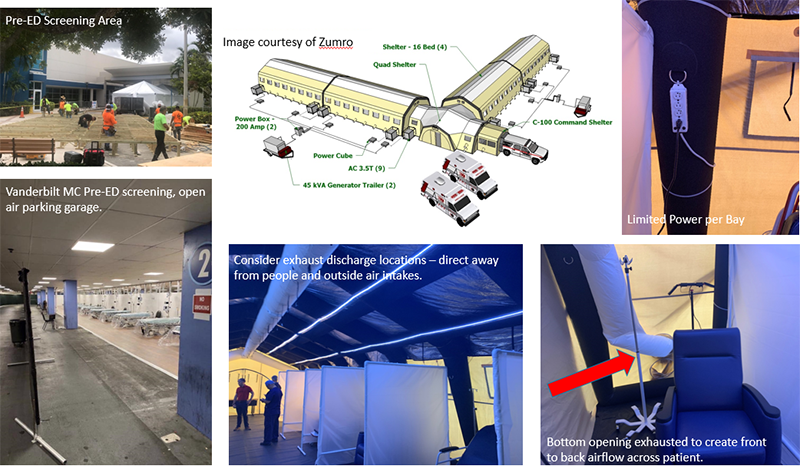
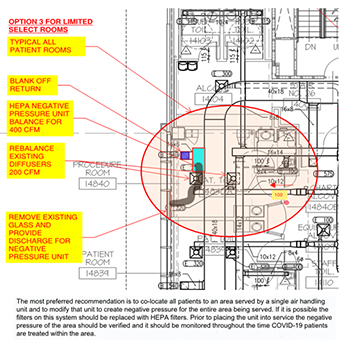
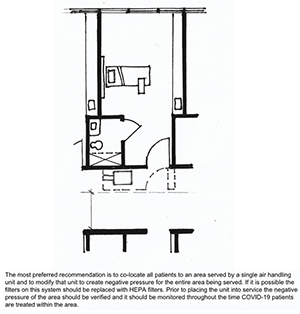
Suggested locations to consider for COVID-19 surge space are listed below. These areas should be considered in relation to the current state of an epidemic. Some areas may not be available for use as facilities reestablish elective services
- Ambulatory Surgery Centers
- Operating Rooms
- Administration areas that used to be patient space
- Consider areas served by the same AHU, on the same floor, within a single “suite”, or within the same smoke zone.
- Images/Concepts for surge space
Concepts for sites, including schools, parking garages, hotels, etc. can be found through this ASHE website: Converting alternate care sites to patient space options
Issues to Plan for and Address:
- Staffing - Adequate Skilled Care Providers and Support Staff
- Supplies - PPE, Beds, Equipment, Infrastructure including HVAC, Power, Internet Access, and Medical Gas
- Space - Site Evaluations and Proximity to Hospital and Areas of Demand
- Do Not Ignore Access to Toilets and Hand Washing (Challenge at Large Volume Spaces Like Convention Centers). Common toilet areas could contribute to transmission and viral load.
- Changes in climate over time that may stress system capacity.
Below are some general parameters for air changes per hour (ACH), temperature, filtration, and relative humidity for non-COVID emergency surge spaces outside of a licensed hospital.
- Minimum 2ACH Outdoor air and 2 ACH Total air, though higher total air is desired (basis is patient room from FGI 1997 ).
- For large volume spaces with high ceilings, such as conference centers, air changes may be calculated based on a ceiling height of 10 feet, however for supply air temperatures above room temperature, minimum OA and total ACH may be calculated as 2ACH Outdoor divided by 0.8 ACH, or 2.5 Total air, (ASHRAE 62.1 ventilation effectiveness) and supply air temperatures kept no more than 15 degrees F above room temperature to minimize stratification and short circuiting of air within the space.
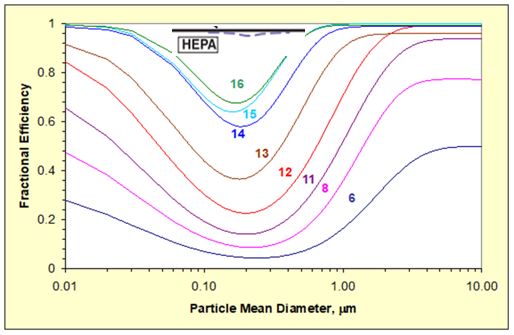
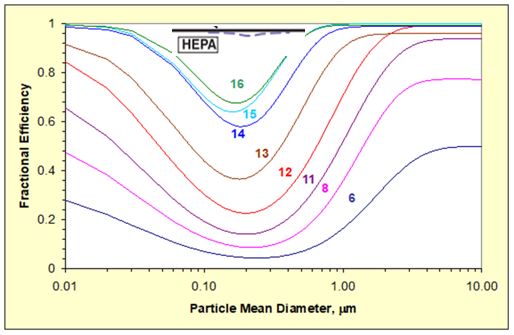
- No less than MERV 13 and MERV 14 preferred for systems that are not serving specialized environments that may require even higher efficiency filtration.
- Temperature 70 – 75 degrees
- Humidity – – consider maintaining 40-60% RH. See additional information here.
- Refer also to Minnesota Department of Health, “Methods for Temporary Negative Pressure Isolation”
Most Basic Approach: Passive Isolation per CDC Guidance*
- One Patient per Room
- Close the Door
- Implement Related CDC Safety Protocols
- Work with clinicians, anticipate patient load, and establish layered approach as needed.
- * Infection Control Recommendations
Strategically Utilize Airborne Infection Isolation Rooms
- Consider utilizing one Airborne Infection Isolation Room for intubation/extubation with one anesthesiologist to conserve PPE
Airflow from Clean to Less Clean
- More important than having to wait a longer time between room changeover due to lower ACH
- More important than air change rate
- More important than outside air % above 2ACH
Increase Filtration Level if Possible
- Consider reduced airflow impacts from higher pressure drop that could lead to loss of desired room pressure differentials. Can the fan be sped up?
- Increase frequency on VFD
- Sheave change if belt driven
- Take care not to allow the fan motor power input to exceed its rated capacity.
- Watch for difficulty with the filter seal due to higher pressure drop across filter.
Guidance on Recirculation and Increased Outside Air Fraction | Return to Top
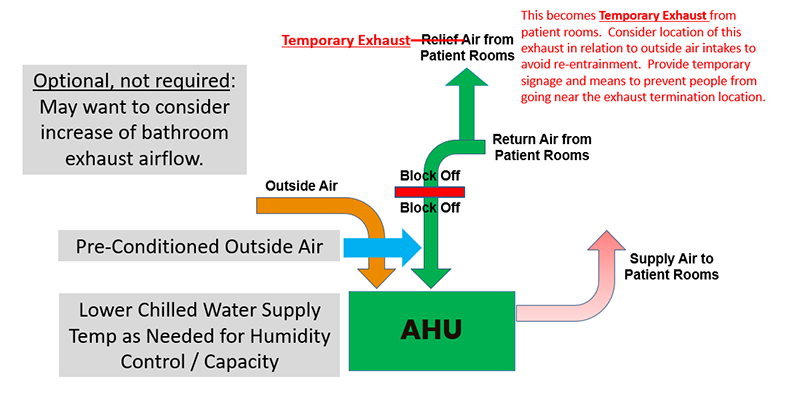
Eliminating recirculation, reducing recirculation, or increasing the outside air fraction are all alternative and optional strategies.
Evaluate recirculation or increasing outside air fraction from design levels up to 100% based on specific surge plan. Where surge plan has increased exhaust air quantities from spaces, increasing the amount of outside air conditioned by the air handler may be necessary to confirm balanced system airflows. Verify room pressures as appropriate. Consider that increasing outside air % may exceed system capacity seasonally and may not be possible without supplementing system capacity and increased energy usage. For systems that already have high levels of filtration (MERV 14 to MERV 16), recirculation can reduce contaminant levels comparably to increasing outside air %. See filter performance information here.
- Protect equipment from freezing – water coils, DX
- Watch for condensation or loss of humidity control
- Consider relaxing temperature setpoints indoors
- Consider future condition when weather becomes more extreme before surge has passed
- Re-confirm ability to achieve desired room pressure differentials
- Watch for operational stability of the fan(s) and adjust to achieve desired airflow
- Adjust frequency on VFD or perform sheave change on belt driven fans.
- Take care not to allow the fan motor power input to exceed its rated capacity.
Consider Maintaining relative humidity at 40-60% RH | Return to Top
Optimal relative humidity continues to be an area of active research.
Suggested Approaches to Deactivate or Bypass Heat Recovery Wheels | Return to Top
Evaluate continued operation of heat recovery wheels.
- Look for these systems in Dedicated Outside Air Units, Energy Recovery Ventilators, and once through units.
- See "Practical Guidance for Epidemic Operation of Energy Recovery Ventilation Systems", authored by ASHRAE TC5.5, including specific Notes on Medical Facilities.
- General Recommendation is that well-designed and well-maintained air-to-air energy recovery systems should remain operating to maintain ventilation, temperature, and humidity levels for maintaining a healthy space.
- During an epidemic, the system should be inspected and evaluated for any possible contribution of zone return air with infectious bioaerosols to the buildings zone supply air.
- Changing operation settings or turning the systems off without an effective understanding of the system will likely have unintended consequences, which may themselves favor the spread of viruses.
Suggested Approaches to Improve/Consider Room Airflow Patterns | Return to Top
Improve/Consider room airflow direction/patterns. When directional airflow is not specifically required, or not recommended as the result of a risk assessment, promote mixing of space air without causing strong air currents that increase direct transmission from person-to-person.
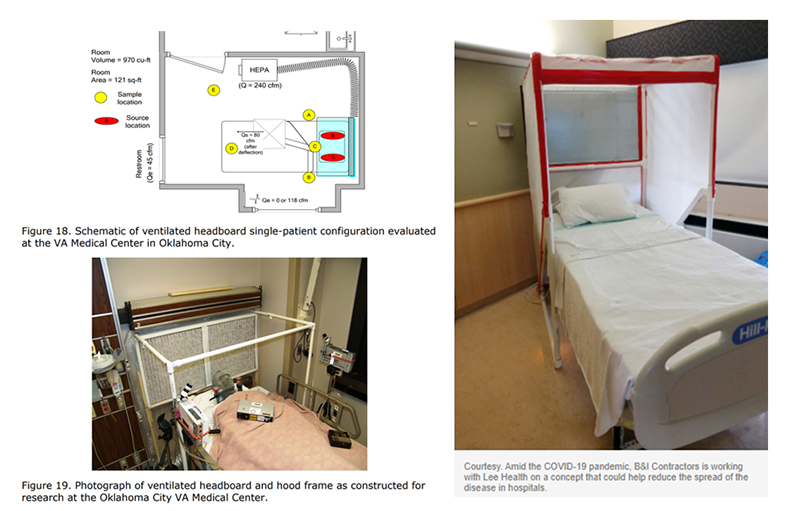
Look at Ventilated Headboards to capture patient-generated aerosols closer to the source. Video from CDC/NIOSH of construction and research validation of ventilated headboard.
- Removal of Airborne Contamination in Airborne Infectious Isolation Rooms.
- Airflow Path Matters: Patient Room HVAC. ASHRAE Journal, vol. 58, no. 6, June 2016.
- CFD Analysis of Hospital Operating Room Ventilation System Part I: Analysis of Air Change Rates. ASHRAE Journal Vol. 60, no. 5, May 2018
- CFD Analysis of Hospital Operating Room Ventilation System Part II: Analyses of HVAC Configurations. ASHRAE Journal, Vol. 60, no. 6, June 2018
- Analysis of Spread Index: A Measure of Laboratory Ventilation Effectiveness. ASHRAE Conference Paper for the ASHRAE Annual Conference, Houston, TX. 2018
Utilize portable ante rooms with HEPA filtration | Return to Top
Portable HEPA MachineWhen We Refer to a “HEPA Unit”, here are some examples:
Ad Hoc Assembly
- HEPA Filter in Frame, Preferably Bag In/Out But As Needed/Available
- Off Shelf Exhaust Fan and Associated Power
- Sealed Connections, Rack or Wheel Mounted

See also the 1-page ASHRAE In-Room Air Cleaner Guidance to Reducing Covid-19 In Air in Your Space/Room
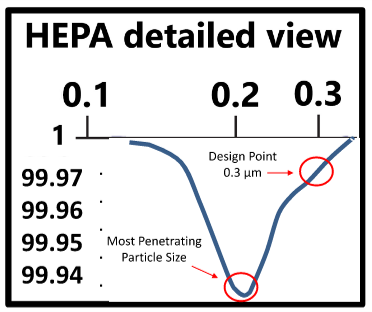
- Yes, individual virus particles can be 0.1 micron or smaller
- Particles and droplets generated by respiration, talking, etc. and by Aerosol Generating Procedures, and possibly toilet flushing are typically much larger than 0.1 micron, making the virus easier to capture.
- By definition, HEPA is at least 99.97% effective for 0.3 micron particles in standard tests (see chart).
- Efficiency is better than MERV 16
- Filters are often delicate and require careful handling to preserve performance.
- HEPA is an effective tool for contaminant removal.

Facilities/Maintenance – PPE | Return to Top
PPE Basics
HVAC System Maintenance and Filter Replacement during the COVID-19 Pandemic | Return to Top
- For HVAC systems suspected to be contaminated with SARS-CoV-2, it is not necessary to suspend HVAC system maintenance, including filter changes, but additional safety precautions are warranted.
- The risks associated with handling filters contaminated with coronaviruses in ventilation systems under field-use conditions have not been evaluated.
- Workers performing maintenance and/or replacing filters on any ventilation system with the potential for viral contamination should wear appropriate personal protective equipment (PPE):
- A properly-fitted respirator (N95 or higher)
- Eye protection (safety glasses, goggles, or face shield)
- Disposable gloves
- Consider letting the filter load up further than usual to reduce frequency of filter changes.
- Don’t let pressure drop increase enough to disrupt room pressure differentials.
- Confirm filters remain snug in their frames.
- When feasible, filters can be disinfected by lightly spraying with a 10% bleach solution or another appropriate disinfectant, approved for use against SARS-CoV-2, before removal. Filters (optionally disinfected or not) can be bagged and disposed of in regular trash.
- When maintenance tasks are completed, maintenance personnel should immediately wash their hands with soap and water or use an alcohol-based hand sanitizer.
Filter Changing in units serving COVID-19 patients | Return to Top
- Consider letting the filter load up further than usual to reduce frequency of filter changes.
- Don’t let pressure drop increase enough to disrupt room pressure differentials.
- Confirm filters remain snug in their frames.
- Follow PPE Basics.
- Turn off AHU if possible. If not possible, consider wearing a bunny suit as additional PPE.
- Virus life on a filter is a function of temperature and relative humidity. Many folks utilize a fixative on the filters before they remove them. Spray with Lysol to disinfect and then use something like hairspray (spray paint works almost as well) to fixate.
- Bag the filter. It’s OK to throw out in regular garbage.
- Guidance for Filtration and Air-Cleaning Systems to Protect Building Environments from Airborne Chemical, Biological, or Radiological Attacks
- Ventilate the Room and Terminal Clean before Re-use
- Follow CDC Air Change Clearance Rates (note these assume perfect mixing):
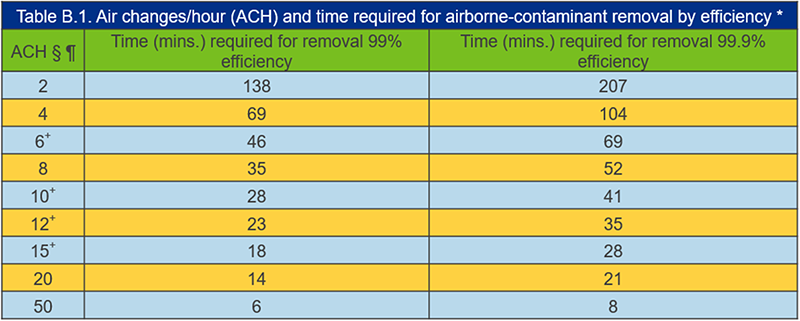
Consider The ASHRAE Equivalent Outdoor Air Calculation, which incorporates the combination of the actual outdoor air, impact of filtration or air cleaning technologies on recirculated air, and the impact of air cleaning technologies in the space.
- Priority on Normal Manual EVS Activities for Terminal Disinfection
- UV Air Cleaning (Note difference between biofouling control vs. virus inactivation)
- UV systems are often installed in air handlers to control biofouling of cooling coils. These systems provide low UV output and are not likely to eradicate virus in the moving airstream. In-duct UV systems can be designed to deliver the necessary dose during the available exposure time to inactivate virus suspended in the air. Such systems require a much higher UV output and are typically designed for 500fpm moving airstream, minimum irradiance zone of 2 feet, minimum UV exposure time of 0.25s, and minimum target UV dose of 1,500 µW·s/cm2. UV light systems should always be coupled with filtration.
- UV-C Disinfecting Lighting
- Upper air UV light fixtures mounted in occupied spaces at heights of 7 ft and above can eradicate airborne SARS-CoV-2 virus. Most direct UV lights are harmful to occupants and furnishings so there are precautions that should be taken during design and installation. Ventilation should maximize air mixing or use supplemental fans for upper room UVC to be more effective. Consider this as an option when there is little or no mechanical ventilation or in congregate settings.
- Bi-Polar Ionization Air Cleaning/Corona Discharge/Needlepoint Ionization and other Ion or Reactive Oxygen Air Cleaners.
- High voltage electrodes create reactive ions in air that react with airborne contaminants, including viruses. A convincing body of scientifically-rigorous, peer-reviewed studies does not currently exist on this emerging technology; manufacturer data should be carefully considered and correspond with the same spplication and occupancy scenario of your intended use. Must comply with UL 2996 and AHSRAE 62.1 as ozone build up can be harmful to humans.
- See ASHRAE Filtration/Disinfection section for information on other technologies such as VHP, Pulsed Xenon, and Chemical Disinfectants.
Coordinate with Clinical Team. Many Hospitals Are Implementing Access Management Plans That Limit Occupancy of Patient Waiting, Including Off-Site Triage Protocols.
- Evaluate Air System Operation and Alternative Measures
- Example: Convert Open Bay or Trauma Room with Use of HEPA Recirculation Unit to Multiple Patient Station
- Example: Convert AHU Temporarily to Once Through Air System; Supplement Make Up Air Needs with Temporary A/C As Needed
- Have a Contingency / Fall-Back Plan
Layered Approach – A Variety of Options | Return to Top
New CDC/NIOSH Info on Expedient Patient Isolation Rooms
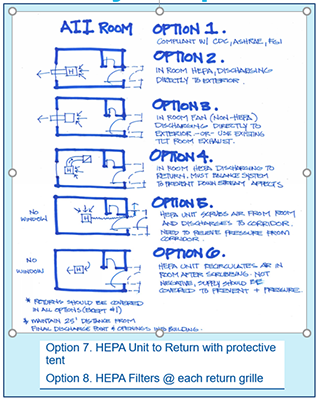
See overview of options 1-6, plus links below to detailed information on these, plus Options 7 & 8. Evaluate what works best for your condition(s).
- Normal Operations – Option 1
- Follow CDC, ASHRAE, FGI Guidelines per your local code.
- Clinical plan may limit airborne infection isolation room use to aerosol generating procedures.
- Small Surge Option: 2 Direct to Outside

- Single patient room with dedicated bathroom
- Seal off return air grill in patient room
- Duct through exterior to the outside.
- Remove window and enclose opening
- Keep door to patient room closed
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor.
- Small Surge: Option 3 HEPA to Outside
- Single patient room with dedicated bathroom
- Seal off return air grill in patient room
- Place HEPA filtered negative air machine in patient room
- Duct through HEPA and then through exterior to the outside.
- Remove window and enclose opening
- Keep door to patient room closed
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor.
- Small Surge: Option 4 – HEPA to Return

- Single patient room with dedicated bathroom
- Place HEPA filtered negative air machine in patient room
- Duct to return air grill
- Seal off remaining part of return air grill
- Verify impact that this will have to the overall air handling system – choosing rooms closest to the air handler may reduce impact
- Keep door to patient room closed
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor.
- Small Surge: Option 5 – HEPA to Corridor
- Single patient room with dedicated bathroom
- Create “airtight” vestibule to patient room
- Need minimum 5’-0” egress clearance in the corridor
- Seal off return air grill in patient room
- Place HEPA filtered negative air machine in vestibule
- Duct through vestibule to corridor
- Keep door to vestibule closed but door to patient room open
- Verify that patient room door is not a rated fire door!
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor.
- Small Surge Option 6 – see image.
- Small Surge: Option 7 – HEPA to Return with Protective Tent
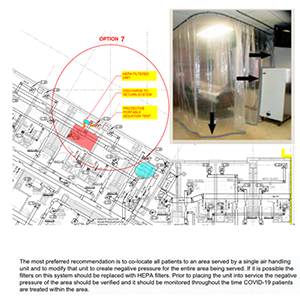
- Single patient room with dedicated bathroom
- Place HEPA filtered negative air machine in patient room
- Install protective portable isolation tent around bed.
- Duct from tent into HEPA and from HEPA into return air grill
- Seal off remaining part of return air grill
- Verify impact that this will have to the overall air handling system – choosing rooms closest to the air handler may reduce impact
- Keep door to patient room closed
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor
- Small Surge: Option 8 – HEPA filter on each return grille, reduce supply to keep room negative to corridor
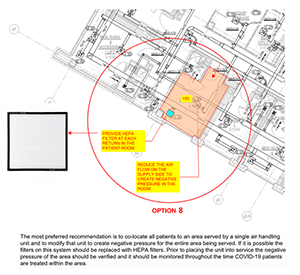
- Single patient room with dedicated bathroom
- Place HEPA filters at each return grille in the room
- Seal off remaining part of return air grill
- Reduce supply air until room is negative to the corridor.
- Verify impact that this will have to the overall air handling system – choosing rooms closest to the air handler may reduce impact
- Keep door to patient room closed
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit patient transport and patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor
Consider Local Exhaust Source Control at Patient Head for Patients on CPAP, Nebulizer, or other AGP.

Ventilated Headboard (can Be Custom Built On Site)
Operating on a COVID-19 patient | Return to Top
- Avoid Use for COVID Patients IF YOU CAN
Additional Info
If You Must:
- Recommend Intubation in Airborne Infection Isolation Room, or if AIIR not available then in Operating Room
- Use Negative Pressure Operating Room if you already have one designed and commissioned for that purpose. Note that ASHRAE Standard 170 no longer includes a negative operating room option.
- Recommend Creating Temporary Vestibule in lieu of Creating a Negative Pressure OR as this is consistent with CDC Guidance (CDC, MMWR December 30, 2005).
- Creates Buffer Zone of Negative Pressure, but maintains OR cleanliness
- Recommend Dedicating an Operating Room for COVID use only
Additional Resources:
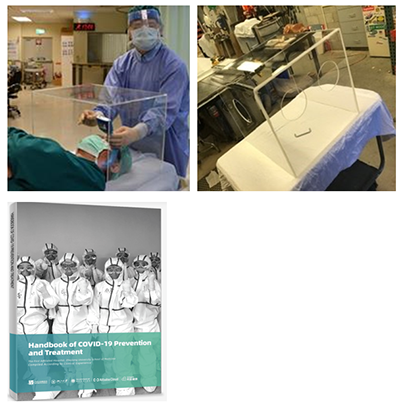
- Intubation Guard
- Built device
- Staff protection
- Use and remove
- Cleanable
- May restrict needed movement
- Seek clinician input first
- Further Guidance
Variable Air Volume Systems | Return to Top
Recognize that VAV Systems Will Vary Airflow Quantity, which presents a risk to maintaining clean to less clean airflow.
- Varying Air Flow Will Hamper Air Balance Goals of COVID Area
IF housing COVID Patients in Area Served by VAV System:
Typical Air Handler w/ Airside Economizer
HVAC – Once through system.
Considerations
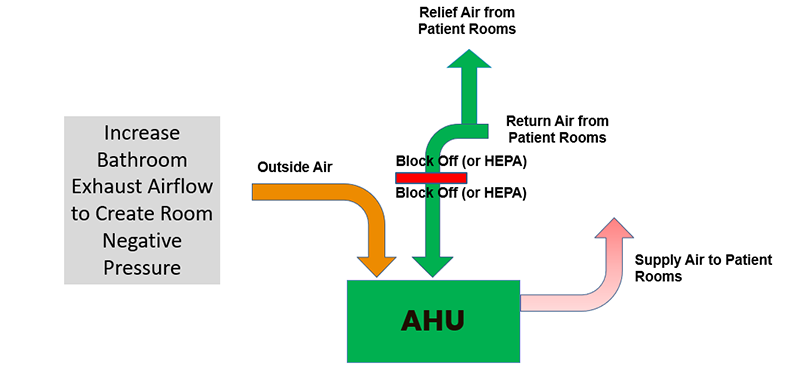
Typical Air Handler w/ NO Airside Economizer
HVAC – Once through system.
Considerations
Room Recirculating Units | Return to Top

There are a variety of in-room recirculating units that utilize decoupled cooling/heating coils:
- Units with moderate filtration due to wetted coil
- Fan Coil Units
- Heat Pump Units including Variable Refrigerant Units
- Package Terminal Air Conditioner (PTAC)
- DX and Mini-Split DX Units
- Units with no filtration requirement (sensible coil)
- Induction Units
- Active Chilled Beams
- The recirculation aspect allows these units to operate at <=6 ACH
View Cautions for rooms with recirculating Units
Caution – Room Recirculating Units | Return to Top
Avoid use for COVID patients if possible, but if you must:
- Consider Option 7 as best layout approach
- If no other option, INCREASE ROOM EXHAUST
- Create negative pressure relative to corridor
- May be accomplished with localized exhaust fan in each room
- Consider system level approach by utilizing increase general or toilet exhaust airflow
- Consider means of sanitizing RR units between patients
- Deep decontamination of RR unit coil after event is over
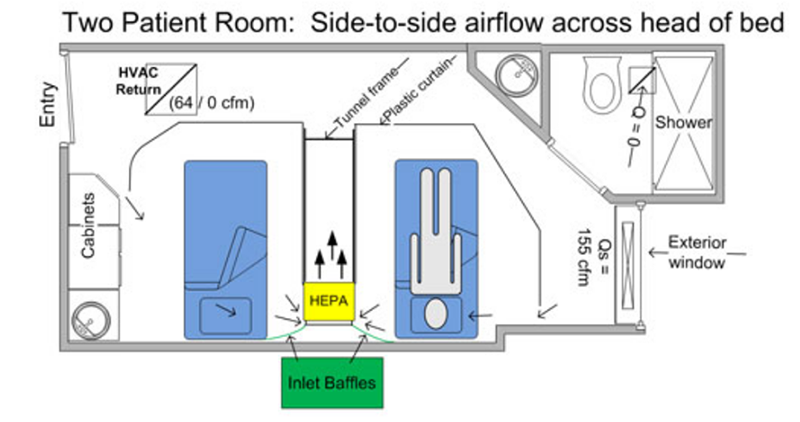
See How-To Document for guidance on creating or managing existing 2-patient rooms.
Cautions when using OR as Temp. ICU | Return to Top
Use of an Operating Room (OR) as COVID-19 Patient Room/Temporary ICU is not ideal, introduces additional risks, and should be considered in relation to the current state of an epidemic. Some areas may not be available for use as facilities reestablish elective services.
- Why? Offers a large space for multiple patients with access to O2, Anesthesia & ventilator machines
- Avoid using OR if possible, but if you must:
- Consider dedicating an OR to COVID patients only or segregate area from remainder of OR suite
- Recommend intubation in Airborne Infection Isolation Room
- Recommend controlled air vestibule in lieu of creating a holistic negative pressure OR, thus creating a buffer zone of negative pressure while maintaining OR cleanliness
- Reduce air changes to 6-12 total ACH
- Modify OA balance to match total/exhaust air.
- Modify capacity for cooling/dehumidification
- All air exhausted from space or HEPA filtered and ducted to return. Label old relief air opening as contaminated exhaust and confirm it will not be re-entrained into OA intakes.
Temporary Vestibule at OR | Return to Top
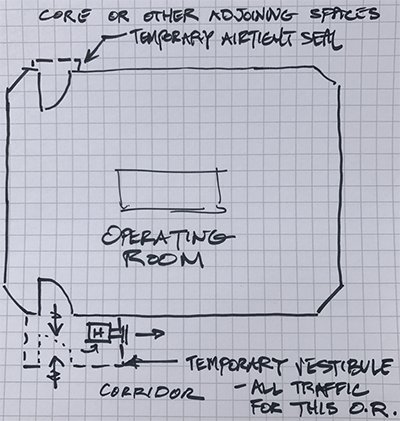
- Example of temporary vestibule to create a negative pressure zone separating OR from corridor
- HEPA unit in vestibule creates negative pressure relationship
- Seal other entries to O.R. to mitigate any contamination potential
Warning on Older ICU Units | Return to Top
Intensive Care Unit (ICU) Rooms
- May operate under positive pressure – verify and address!
- Must operate under negative pressure
- Designate specific room(s) and area(s)
- Proactively review and modify test and balance as needed
- Consider system level, once air approach is determined
- Changing OA volume may impact building pressure balance
- Monitor humidity effects due to system changes
- All air exhausted from space or HEPA filtered and ducted to return
Gastrointestinal Endoscopy | Return to Top
Suggested Approach for Endoscopy Procedures
- ASHRAE Standard 170 requires 6 total ACH for Gastrointestinal Endoscopy procedure rooms. There is no pressure requirement. Airflow may not be recirculated within the room.
- Be aware that pressure relationships for Endoscopy rooms have changed over the years. Re-confirm facility operating condition.
- Test patients for COVID-19. Patients who test positive should have their procedure delayed until following recovery, if possible.
- If the procedure is an aerosol generating procedure, regardless of whether it is on a COVID-19 positive patient or not, perform the procedure in an airborne infection isolation room or a bronchoscopy room.
- ASHRAE Standard 170 requires 12 total ACH for Bronchoscopy rooms. The room must be negative, 100% exhaust, and no recirculation within the room.
- If the procedure is not aerosol generating, patient is COVID-19 positive or unknown and procedure can not be delayed then recommend these options, in order
Transmission through Air in Toilet Rooms and into patient rooms | Return to Top
Studies have shown that toilets can be a risk of generating droplets and droplet nuclei "plumes" into the air that could contribute to transmission.
- Keep toilet room doors closed, even when not in use
- Put the toilet seat lid down, if there is one, before flushing1
- Confirm that fan is operating
- Hospital airborne C-Difficile Study2
- C-Diff seeded in a toilet
- Water samples, settle plates, and air samples
- Spores present after 24 flushes
- Droplet nuclei spore bioaerosol produced over at least 12 flushes

1. Best, EL et.al Potential for aerosolization of Clostridium difficile after flushing toilets: the role of toilet lids in reducing environmental contamination risk 2012 J Hosp Infect
2. Johnson, David Mead, Kenneth et.al Toilet Plume Aerosol Generation Rate and Environmental Contamination Following Bowl Water Inoculation with Clostridium difficile Spores 2019 American Journal of Infection Control
Johnson, David Mead, Kenneth et.al. Lifting the Lid on Toilet Plume Aerosol: A Literature Review with Suggestions for Future Research 2013 American Journal of Infection Control
Waterborne Pathogen Prevention | Return to Top
- When an area of a hospital or medical facility is reopened for use, water systems in these spaces should be evaluated in their entirety following the facility's water management plan. This may include flushing and testing for waterborne pathogens, drainage system borne pathogens, etc. prior to occupancy, and subsequent control measures discussed, if needed, to prevent HAI's.
- Due to changing municipal water usage declining (i.e. older water with less disinfectants in it), hospitals should consider testing the incoming water for disinfectant and bacteria to determine if their incoming water quality is worsening.
- Water usage inside the facility may change and thus new waterborne pathogen hot spots may develop. Hospital facilities should consider additional flushing where low use may occur.
- Carefully consider changes to the system. For example, changing to hands free (sensor) faucets to minimize contact potential may result in increased water age, requiring piping modifications.
- Maintaining the cleanliness of fixtures, especially those that can produce aerosols, like shower heads and faucet aerators, will mitigate exposure to waterborne pathogens. Having cleaning procedures in place for water-aerosolizing fixtures can help reduce exposure.
- Additional resources:
Demand for Gasses in ICU Rooms
- Oxygen (O2).
- Typically fitted out with three (3) outlets for a total flow of about 1.0 scfm plus ventilator demand
- Ventilators deliver gas to a patient based on their respiration rate and their lung capacity
- Ventilators can consume 100% MS-AIR (w/ 21% oxygen) and no O2 all the way up to 0% MS-AIR and 100% O2 depending on the ability of lungs to exchange gasses in the blood
- Gross O2 demand adds up to a range of 2.0-2.5 scfm
- Medical-surgical compressed air (MS-AIR)
- Typically fitted out with one (1) outlet for a total flow of about 1.0 scfm plus ventilator demand
- Gross MS-AIR demand adds up to a range of 2.0-3.0 scfm
- Ventilators
- Multiple patients serviced by a common ventilator is not recommended by medical officials for a variety of reasons
Demand for Gasses in Med-Surg Rooms and ORs
- Medical-surgical patient rooms
- These rooms have insufficient # of O2 and MS-AIR outlets, but their local piping connections may be sufficient to handle ventilators for certain clinical cases; they’d be sufficient for those patients who need O2, but don’t need a ventilator to breathe for them.
- Operating rooms
Note that use of an Operating Room (OR) as COVID-19 Patient Room/Temporary ICU is not ideal, introduces additional risks, and should be considered in relation to the current state of an epidemic. Some areas may not be available for use as facilities reestablish elective services.
- OR’s become options because they are fitted out with O2 and MS-AIR in sufficient capacity to allow the use of anesthesia machines as ventilators (the ASA has guidance).
- Using an OR as an Airborne Infection Isolation room creates a problem with the area alarms because of the location of the pressure sensor. Consider “fire watch” type monitoring of zone valve boxes.
- Using an OR temporarily as an Airborne Infection Isolation room will require that pressurization be addressed including ante-rooms and exhaust for the room itself (could use a dedicated smoke exhaust if the suite is fitted out with such a system).
Accommodating increased demand (flow) in fixed piping systems
- Raising system pressure in O2 systems
- Raise pressure up to 55 psig if not set there already
- Supplier may need to do this because the regulator is within the bulk plant enclosure
- Can be done by facility staff at manifolded sources
- Re-calibrate area alarm panels
- Raising system pressure in MS-AIR systems
- Rise pressure up to 55 psig if not set there already
- Can be done by facility staff at compressor sets or manifolded sources
- Re-calibrate area alarm panels
- Reducing pressure drop through the piping
- Provide temp O2 and/or MS-AIR sources near ICU suite
- Provide temp ICU rooms closer to existing sources
Impact of demand/consumption on existing gas systems
- O2 systems
- More rapid and increased O2 consumption leads to more ice buildup on vaporizer; de-icing service critical. Consider use of portable fans or misters to reduce ice build-up on vaporizers.
- Ensure bulk supplier can make more frequent deliveries
- Ensure supplier can make more cylinder/container exchanges
- Test your LPEOSC to ensure that it’s in working order
- Consider using your LPEOSC as a means by which more product can be introduced into the existing piping
- MS-AIR systems
- Increased demand and consumption may result in standby compressors operating; consider adding another receiver as a buffer
- Longer run times could result in compressors and/or motors overheating; consider better ventilation of equipment room or spot cooling
- Ensure supplier can make more cylinder/container exchanges
Consider providing supplementary gas sources
- Provide auxiliary source connection at bulk plants per NFPA 99 (new requirement in the 2015 edition)
- Mitigates the use of the LPEOSC as more than just a short-term, interim source
- Provide additional LPEOSC
- Strategically located in case the other LPEOSC is obstructed for some reason; interconnection critical
- Provide in building emergency reserve (IBER) as defined by NFPA
- This can be manifolded sources of high pressure gas (cylinders) or high pressure liquids (containers) for O2 and/or MS-AIR
- Ensure that new storage rooms have enough space, have product secured safely and are properly ventilated properly
- Provide redundant vacuum and compressor sets
- Careful interconnection required
Below are the members of the Healthcare Team of the Epidemic Task Force
| Traci Hanegan (Chair) |
Coffman Engineers, Inc. |
| Robert Block |
Dr. Robert M. Block, DDS |
| Mike Cummiskey |
Virginia Dept. of Health/Dental Division |
| Tim Earhart |
McDonough Bolyard Peck |
| David Eldridge |
Grumman/Butkus Associates |
| Jeremy Fauber |
Heapy |
| Jonathan Flannery |
ASHE |
| Melvin Glass |
EMC Engineers |
| Eric Granzow |
Specialized Engineering Solutions |
| Rick Hermans |
Retired |
| Jerry Ivey |
Willis-Knighton Health System |
| Roger Lautz |
Affiliated Engineers Inc. |
| Mike Meteyer |
Erdman |
| Frank Mills |
Frank Mills Consulting |
| Zaccary Poots |
Toro-Aire Inc |
| Michael Sheerin |
TLC Engineering Solutions |
| Wayne Stoppelmoor |
Schneider Electric |
| Paul Supan |
American Dental Association Volunteer |
| Steven Welty |
Green Clean Air |
| Laurence Wilson |
WSP |
Thanks to the following people who, along with members of the Healthcare Team, provided input, information and review of the materials in the development of documents.
| Jane Rohde |
JSR Associates, Inc. |
| Kara Brooks |
ASHE |
| Mark Costello |
TLC Engineering Solutions |
| Bob Danner |
TLC Engineering Solutions |
| Jim Ferris |
TLC Engineering Solutions |
| Aaron Johnson |
TLC Engineering Solutions |
| Nicole Johnson |
Coffman Engineers, Inc. |
| Christoph Lohr |
ASPE |
| Ken Mead |
ASHRAE TC9.6 Healthcare Facilities |
| Luca Piterà |
AICARR |
| Ben Roseborough |
TLC Engineering Solutions |
| Kevin Scarlett |
Washington State Department of Health |
| Jeff Stone |
TLC Engineering Solutions |
| John Williams |
Washington State Department of Health |
This ASHRAE/ASHE guidance document is based on best available evidence and knowledge as of the date of this document. In the context of the rapidly evolving state of knowledge regarding transmission of COVID-19, design professionals may consider interventions that adopt a precautionary principle, taking reasonable actions that reduce risk while awaiting greater scientific certainty. Therefore, this guidance should be read in conjunction with the relevant government guidance and available research. This material is not a substitute for the advice of a qualified professional. By adopting these recommendations for use, each adopter agrees to accept full responsibility for any personal injury, death, loss, damage or delay arising out of or in connection with their use by or on behalf of such adopter irrespective of the cause or reason therefore and agrees to defend, indemnify and hold harmless ASHRAE and ASHE, the authors and others involved in their publication from any and all liability arising out of or in connection with such use as aforesaid and irrespective of any negligence on the part of those indemnified.