Facilities of Concern | Modes of Transmission | Airborne Transmission | Aerosol Generating Procedures | Secondary Infection Susceptibility | Resident Protection -Employee/Staffing/Partners | Surface Cleaning and Disinfection | Suggested Approaches | HVAC Strategies for LTC Infection Management & Prevention | Filtration | Air Cleaning | Air Pressure – Protect or Isolate | COVID Resident or Patient: HEPA to Corridor | Room Recirculating Units | Caution – Room Recirculating Units | 2-Person Resident or Patient Room | Source Control Options | Suggested Approaches | Transmission Through Air in Toilet Rooms | Consider Maintaining 40-60% RH | Facilities/Maintenance – PPE | HVAC System Maintenance and Filter Replacement during the Pandemic | Filter Changing in units serving COVID-19 residents/patients | Facilities / Maintenance | New Facility Design Considerations | Acknowledgements
This document is intended for the following facility types:
- Long Term Care / Extended Care
- Assisted Living
- Nursing Home
- Hospice
- Memory Care
- Post acute
The background for residential health, care, and support facilities as referenced in the Facility Guidelines Institute’s Guidelines for Design and Construction of Residential Health, Care, and Support Facilities include long term care / extended care settings. The guidance information provided comes from various sources and it is important to note that coupling both operational policies and procedures with design interventions can contribute to better overall outcomes for residents, patients, staff, and families.
- SARS-CoV-2, the virus that causes COVID-19, is thought to spread mainly from person-to-person through respiratory droplets. Recent research indicates that SARS-CoV-2 is resilient in aerosol form and may be a more important exposure pathway than previously considered.
- Infectious respiratory droplets/aerosols are produced when an infected person talks, coughs or sneezes.
- Droplets can land in the mouths or noses of nearby people.
- Droplets can land on surfaces and be spread through contact with contaminated surfaces.
- When in close contact with an infected person, aerosols/droplet nuclei can possibly be inhaled into the lungs.
- Recognize that SARS-CoV-2 may be aerosolized during Toilet Flush
- Considerations
- Keeping plumbing traps full of water to avoid transmission of air through dry traps.
- SARS-CoV-1 has been shown to be transmitted this way, however it is not yet known or confirmed if SARS-CoV-2 can be transmitted in a similar manner.
- See the following reference documents:
ASHRAE Statement on airborne transmission of SARS-CoV-2:
- Transmission of SARS-CoV-2 through the air is sufficiently likely, therefore airborne exposure to the virus should be controlled.
- Changes to building operations, including the operation of HVAC systems can reduce airborne exposures.
ASHRAE Statement on operation of heating, ventilating, and air-conditioning systems to reduce SARS-CoV-2 transmission:
- Ventilation and filtration provided by heating, ventilating, and air-conditioning systems can reduce the airborne concentration of SARS-CoV-2 and thus the risk of transmission through the air.
- Unconditioned spaces can cause thermal stress to people that may be directly life threatening and that may also lower resistance to infection.
- In general, disabling of heating, ventilating, and air-conditioning systems is not a recommended measure to reduce the transmission of the virus.
Aerosol Generating Procedures | Return to Top
It is possible that the virus is spread through aerosol, so minimize aerosol generating procedures or use engineering methods to adequately control their generation at the source.
- Positive pressure ventilation (BiPAP and CPAP)
- Nebulizer treatment
The number of occupants in a room should be kept to a minimum during aerosol generating procedures.
Secondary Infection Susceptibility | Return to Top
Secondary infections are a significant complicating factor for residents/patients with COVID-19. There are studies that show a significant portion of individuals with COVID-19 also acquire another infectious disease.
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- This study showed how developing a co-infection (secondary infection) from a hospital when a patient is dealing with COVID-19 increases the likelihood of death by 27 times.
- Precautions are Needed for COVID-19 Patients with Coinfection of Common Respiratory Pathogens
- Among COVID-19 patients in Qingdao, 80.00% of them had IgM antibodies against at least one respiratory pathogen, whereas only 2.60% of the patients in Wuhan had positive results for serum IgM antibody detection. The most common respiratory pathogens detected in Qingdao COVID-19 patients were influenza virus A (60.00%) and influenza virus B (53.30%), followed by mycoplasma pneumoniae (23.30%) and legionella pneumophila (20.00%). Legionella Pneumophila is a waterborne pathogen from the plumbing system and needs to still be addressed.
- Co-infection with SARS-CoV-2 and Influenza A Virus in Patient with Pneumonia, China - reported co-infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and influenza A virus in a patient with pneumonia in China.
- The case highlights possible co-detection of known respiratory viruses. Low sensitivity of upper respiratory specimens for SARS-CoV-2 could further complicate recognition of the full extent of disease.
Resident Protection -Employee/Staffing/Partners | Return to Top
- Increased use of touchless sensors
- Increase high touch surface cleaning disinfection
- Provide areas for staff donning/doffing
- Provide areas for staff respite
- Provide area for separate screening/entry of staff and/or visitors
- CDC Guidelines: Plan, Prepare, and Respond
- Refer to the AMDA references (The Society for Post-Acute and Long-Term Care Medicine) for additional resident protection guidance, resources, & tools
Surface Cleaning and Disinfection | Return to Top
Materials and Surface – COVID-19
Information on SARS–CoV–2 (virus) and COVID-19 (disease)
SARS-CoV-2 is a positive sense, single stranded enveloped RNA virus and is relevantly easy to kill by impacting the lipid envelop structure which is easily compromised by disinfectants. Once envelope is damaged, the virus is compromised and is no longer able to infect humans¹.
In selecting a disinfectant, there are considerations for which disinfectant to use to kill the virus:
- Be the least caustic in relationship to the environmental services technicians or end user handling, mixing, and/or using the disinfectant chemical.
- The potential of the material or surface being cleaned and disinfected and the potential of material degradation because of the use of the disinfectant chemical. Verify with both disinfectant chemical manufacturer and material/surface product manufacturer.
- Selected disinfectant and chosen application method should be listed on EPA’s List N: Disinfectants for Use Against SARS-CoV-2 (COVID-19)
¹Cascella M, Rajnik M, Cuomo A, et al. Features, Evaluation and Treatment Coronavirus (COVID-19) [Updated 2020 Apr 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 January: available online at https://www.ncbi.nlm.nih.gov/books/NBK554776/ Schoeman, D., Fielding, B.C. Coronavirus envelope protein: current knowledge. Virol J 16, 69 (2019): available online at https://doi.org/10.1186/s12985-019-1182-0
Surface Cleaning and Disinfection
Environmental Materials and Surface Types – Noncritical Items
Centers for Disease Control and Prevention: 3 categories of items and surfaces related to cleaning and disinfection within healthcare settings. The type of item determines the level of disinfectant required².
Critical Items – confers a high risk of infection if contaminated with any microorganism; this category includes surgical instruments, and anything inserted within a sterile tissue or body cavity.
Semicritical Items – makes contact with mucous membranes or nonintact skin; this category predominantly includes medical devices.
Noncritical Items – makes contact with intact skin but not mucous membranes; this category is divided into noncritical patient care items (i.e. bedpans, blood pressure cuffs, computers, etc.) and noncritical environmental surfaces (i.e. bedside table, nurse call buttons, TV remote, patient furniture, floors, etc.).
²Reference: CDC, A Rational Approach to Disinfection and Sterilization: Guideline for Disinfection and Sterilization in Healthcare Facilities (2008)
Surface Cleaning and Disinfection
Materials and Surfaces - Disinfecting High Touch Surfaces
Cleaning and Disinfection – EPA Registered Disinfectants
Surface cleaning to remove dust, soil, blood, etc. is required prior to disinfecting to maximize achievement of efficacy.
Disinfectants for environmental surfaces are included in the United States Environmental Protection Agency List “N”, an ever-evolving list of disinfectants, applicable surface types, and application methods that are deemed effective against SARS-CoV-2 virus that causes COVID-19 (no EPA endorsement).
High tough point surfaces mean items that are touched by the human hand – these are called “fomites” – such as doorknobs, handrails, TV remotes, nurse call, countertop, etc.
Flooring is considered a surface requiring low level disinfection because of the risk of cross contamination between rooms – need for frequent solution changes, mop head and microfiber laundering, etc. If an object falls on the floor, i.e. TV remote and is picked back up – could spread disease if not cleaned and disinfected prior to being handed back to resident.³
³Reference: CDC, A Rational Approach to Disinfection and Sterilization: Guideline for Disinfection and Sterilization in Healthcare Facilities (2008)
4CDC Resource Page last reviewed: May 7, 2020 Content source: National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases
Material Selections and Considerations
Unintended Consequences: Use of disinfectants on existing materials and surfaces may cause degradation of the product. Request information from disinfectant chemical manufacturer and product manufacturer for verification.
Product Performance: replacement for products that are high touch points – evaluate non-porous materials that can withstand cleaning and disinfection – upholstery, arm caps and chair arms, solid surface countertops, resilient flooring, etc.
Product Characteristics: evaluate acoustical needs and address on walls, ceilings, and other surfaces that can be laundered and/or cleaned and sanitized as soft, porous surfaces that are not high touch surfaces or in high traffic areas requiring disinfection.
Product Aesthetic: In selecting surfaces for long term care – an understanding that the aesthetic should reflect the feeling of home or a residence is a consideration for product selection. A person lives in a residential care setting because of a diagnosis, but the person is not the diagnosis, but an individual living in space that needs as comfortable and homelike as possible.
Emerging Technologies – Evaluation Underway
If ANY emerging technology is used in a residential care facility, all precautions must be taken for those with and without cognitive impairment, as rooms can not be occupied when using this methods for disinfection.
Electrostatic Sprayers⁵
Used as an application method with EPA List N Registered Disinfectant. Because effectiveness is uncertain it needs to be vetted with chemical manufacturer, product/surface manufacturer, and impact to environmental services technician / end user with appropriate PPE.
Portable Ultraviolet C Units (UV-C)⁶
Some hospitals utilize UV-C as an additional disinfection method beyond physical cleaning and chemical disinfection. Typically materials are not minimum performance tested for the accumulative impact of UV-C on materials that have been cleaned and disinfected, but not rinsed. However, there has been efficacy from a disinfection perspective.
⁵EPA, New Releases from Headquarters, Office of the Administrator (AO), Office of Policy (OP): EPA Expands Research on COVID-19 in the Environment (04/20/2020): available online at https://www.epa.gov/newsreleases/epa-expands-research-covid-19-environment
⁶Guridi, A., Sevillano, E., de la Fuente, I., Mateo, E., Eraso, E., & Quindós, G. (2019). Disinfectant Activity of A Portable Ultraviolet C Equipment. International journal of environmental research and public health, 16(23), 4747: available online at https://doi.org/10.3390/ijerph16234747
Most Basic Approach: Passive Isolation per CDC Guidelines
- One Resident per room.
- Close the door.
- Implement relevant CDC Safety Protocols.
- Evaluate measures to reduce isolation and interaction – technology, window visits and other similar strategies for engagement.
COVID-positive residents
- COVID positive residents represent a transmission risk to other residents and staff as well as being a vulnerable person to additional diseases; therefore communities should try to address both of these risks in their care approaches.
- Dedicated COVID-19 unit is recommended
- Transfers from within facility for COVID positive.
- Admissions/readmissions from hospitals for COVID positive.
HVAC Strategies for LTC Infection Management & Prevention | Return to Top
Potential Strategies / Opportunities
- Improve level of filtration.
- Utilize/create relative air pressure differences to direct airflow.
- Increase dilution by increasing outside air.
- Utilize directional airflow and local source control techniques.
Evaluate for Resident Rooms & Common Areas
- Different equipment and systems – centralized versus decentralized.
- Different opportunities and challenges.
Prevent recirculation of the lighter particles
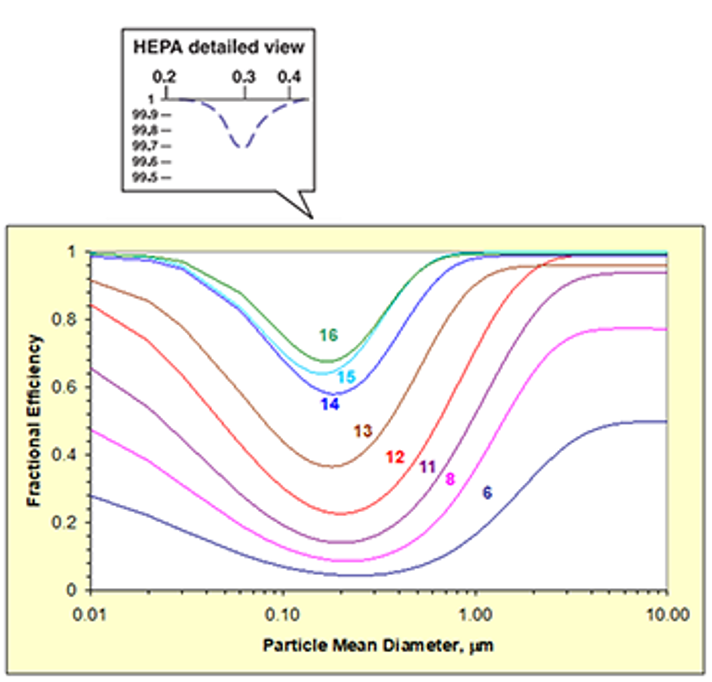
Mechanical Air Filters
Consist of media with porous structures of fibers or stretched membrane material to remove particles from airstreams.
Some filters have a static electrical charge applied to the media to increase particle removal.
The fraction of particles removed from air passing through a filter is termed “filter efficiency” and is provided by the Minimum Efficiency Reporting Value (MERV) under standard conditions.
Increased filter efficiency may result in increased pressure drop or reduced airflow through the filter. Try to utilize higher efficiency filters with similar pressure drop or verify HVAC systems can handle filter upgrades without negative impacts to pressure differentials and/or air flow rates prior to changing filters.
Generally, particles with an aerodynamic diameter around 0.3 μm are most penetrating; efficiency increases above and below this particle size.
Overall effectiveness of reducing particle concentrations depends on several factors:
- Filter efficiency
- Airflow rate through the filter
- Size of the particles
- Location of the filter in the HVAC system or room air cleaner
It is critical to wipe the wires in electrostatic precipitators as silicone buildup reduces efficiency.
Always follow manufacturer’s instructions when using electronic air filters.
For more information, see the ASHRAE Position Document on Filtration and Air Cleaning.
Increase Filtration Level if Possible
- Most valuable for recirculated air
- Investigate reduced airflow impacts from higher pressure drop
Resident Room HVAC Equipment – filter options limited
- Many recirculation unit filters have no or low MERV rating
Air Cleaning (Disinfection/Sterilization of Air)
UVGI
The use of Ultraviolet Light for Germicidal Irradiation has been known about for a long time. In fact, the ability of sunlight to prevent microbial growth – to inactive micro-organisms – was first identified in 1877 by Downes and Blunt (1). There have been many further research applications since then and UV has been of interest whenever an airborne infectious disease becomes active in a community.
For example, the use of UV to sterilize air became popular as a way of limiting TB spread since the 1980 and has since become an accepted method of ‘air cleaning’ in many countries, notably in North America and Asia where a range of products are available.
REDUCING INFECTION RISK USING LOCAL UVGI AIR DISINFECTION
There are 2 options for local units….
- Upper room units installed high up on a wall, in a ceiling, or free hanging at high level
- Mobile floor mounted units which can be wheeled into position.
Upper room - UVGI
Inside rooms, upper room (ceiling void) UVGI – Ultra Violet Germicidal Irradiation units –could be installed into a false ceiling as a recessed unit (usually about 12 inches depth) or if no ceiling then installed to hang at a height of about 8 to 9 ft .
The units are typically 24 inches x 24 inches so that they can be installed into a standard ceiling grid. Each unit draws in air and passes it across UV lamps – which are hidden from direct view inside the unit box – and effectively ‘kill’ viruses by breaking their DNA so that the virus cannot replicate.
A single unit could achieve acceptable risk reduction in a resident’s room or other small room such as an office.
These type of upper room UVGI units have “supply air jets” so room layout considerations should take into account any drafts that could affect thermal comfort and how to remove stagnant air areas within the space.
A UVGI unit could be very useful in an elevator because it would draw air through and control the viral load in the elevator. Although full elevator occupancy would still not be advisable, elevators could transport more than one depending on capacity. It is normal practice for a caregiver to accompany a resident in an elevator and this solution would assist and would be greatly better than the 1 person per elevator recommendation currently necessary to meet social distancing rules.
Ceiling jets can be used in any other ‘hot spots’ to reduce viral load.
It is recommended that for maintenance purposes units are simply removed and taken away for cleaning, lamp replacement or any other maintenance function and a new unit installed in its place. This would avoid any loss of resident room.
IN DUCT UV AIR CLEANING
For buildings with central AHU ventilation plant, the use of in duct UV can be considered and should be developed as a solution by a HVAC engineer.
UV air cleaning units can be installed at the central plant and/or in branch ducts. The location must allow access for safe removal and replacement of lamps.
In order to achieve maximum dwell times the lamps should run parallel with the air flow rather than perpendicular to it. This will ensure that dwell times and proximity to the lamp surfaces are achieved in order to kill viruses effectively.
UV light is hazardous to humans and should be obscured.
Whatever type of UVGI unit is used it is imperative that the UV light does not shine into the occupied space and is not visible. Manufacturers provide units which fully enclose the UV lamps, and have facilities to easily remove for replacement or cleaning safely but only when the lamps are off.
This ensures the lamps are not visible to humans. The lamps are positioned to have close contact with the air borne particles and sufficient dwell time to ‘kill’ the virus. UV intensity and dwell time are necessary for effective virus kill rates.
Resources and references
¹On the influence of light upon protoplasm, Arthur Downes, Thomas P. Blunt, Published:01 January 1879 https://doi.org/10.1098/rspl.1878.0109
²Upper-Room Ultraviolet Light and Negative Air Ionization to Prevent Tuberculosis Transmission, Escombe et al, Department of Infectious Diseases & Immunity, Imperial College London, United Kingdom, 2008
³ASHRAE Handbook Applications 2019 Chapter 62 Ultraviolet Air and Surface Treatment
⁴Illuminating Engineering Society IES Committee Report: Germicidal Ultraviolet (GUV), IES CR-2-20-V1
Emerging Technologies
Photocatalytic Oxidation (PCO)
Consists of a pure or doped metal oxide semiconductor material
Most Common Photocatalyst is Ti02 (titanium dioxide)
Activated by a UV light source
UV-A (400-315nm)
UV-C (280-200nm
UV-V (under 200nm) Ozone can be formed at UV-V wavelengths
Light mediated, redox reaction of gases and biological particles absorbed on the surface
Some units claim disinfection from gaseous hydrogen peroxide.
Possible by-products formed by incomplete oxidizing.
Some air cleaners using PCO remove harmful contaminants to levels below limits for reducing health risks set by recognized cognizant authorities.
Some are ineffective in reducing concentrations significantly; manufacturer data should be considered carefully.
For more information, see the ASHRAE Position Document on Filtration and Air Cleaning.
Bipolar Ionization/Corona Discharge
- High voltage electrodes create reactive ions in air that react with airborne contaminants, including viruses.
- The design of the corona discharge system can be modified to create mixtures of reactive oxygen species (ROS), ozone, hydroxyl radicals and superoxide anions.
- Systems are reported to range from ineffective to very effective in reducing airborne particulates and acute health symptoms.
- Convincing scientifically-rigorous, peer-reviewed studies do not currently exist on this emerging technology; manufacturer data should be carefully considered.
- Systems may emit ozone, some at high levels. Manufacturers are likely to have ozone generation test data. Must comply with UL 2996 and ASHRAE 62.1 as ozone build up can be harmful.
Air Pressure – Protect or Isolate | Return to Top
Consider opportunities to modify the air flow direction
- Resident Rooms => positive air pressure to protect residents
- Resident Positive Infection Rooms with HEPA to Corridor => resident room positive air pressure to HEPA unit, negative air pressure to corridor
- Resident Positive Infection Rooms and/or Isolation Wings => negative air pressure
- Pressure difference should be demonstrable by direction of airflow such as from a tissue being moved from air transfer at the cracks of a closed door or other similar approach
COVID Resident or Patient: HEPA to Corridor | Return to Top
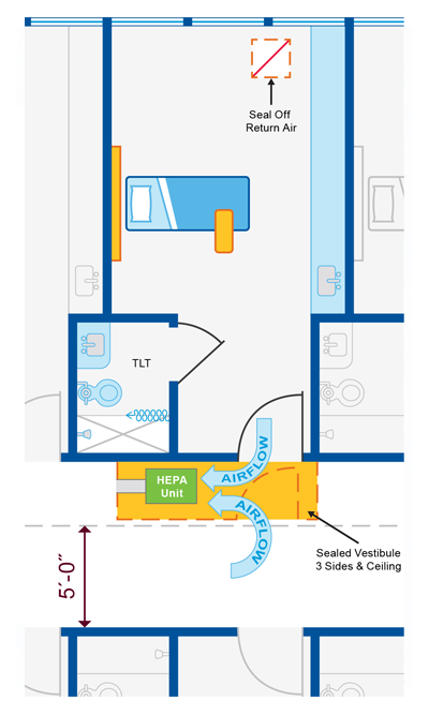
- Goal: Create a room that protects high risk resident/patient with positive room pressure and protects other high-risk resident/patients with negative anteroom.
- Single resident or patient room with dedicated bathroom
- Create “airtight” vestibule to room
- Need minimum 5’-0” egress clearance in the corridor
- Seal off return air grill in room
- Place HEPA filtered negative air machine in vestibule
- Duct through vestibule to corridor
- Keep door to vestibule closed but door to resident/patient room open
- Verify that room door is not a rated fire door!
- Verify negative pressure prior to placing room in service and monitor negative pressure while in service
- Limit resident/patient transport and resident/patient transfers
- Terminal cleaning after ACH removes potentially infections particles
- Notify Healthcare workers that HEPA units can not be turned off once in place as this may result in an unsafe condition with the room becoming positively pressurized to the corridor.
The most preferred recommendation is to co-locate all patients to an area served by a single air handling unit and to modify that unit to create negative pressure for the entire area being served. If it is possible the filters on this system should be replaced with HEPA filters. Prior to placing the unit into service the negative pressure of the area should be verified and it should be monitored throughout the time COVID-19 patients are treated within the area.
Room Recirculating Units | Return to Top

There are a variety of in-room recirculating units that utilize decoupled cooling/heating coils:
- Units with low to moderate filtration due to wetted coil
- Fan Coil Units
- Heat Pump Units
- Package Terminal Air Conditioner (PTAC)
- DX and Mini-Split DX Units
- Units with no filtration requirement (sensible coil)
- Induction Units
- Active Chilled Beams
- The recirculation aspect allows these units to operate at <=6 ACH
Cautions for rooms with recirculating units
Caution – Room Recirculating Units | Return to Top
Avoid use for COVID residents and patients if possible, but if you must:
- Consider HEPA to Corridor as best layout approach
- If no other option, increase room exhaust
- Create negative pressure relative to corridor
- May be accomplished with localized exhaust fan in each room
- Consider system level approach by utilizing increase general or toilet exhaust airflow
2-Person Resident or Patient Room | Return to Top
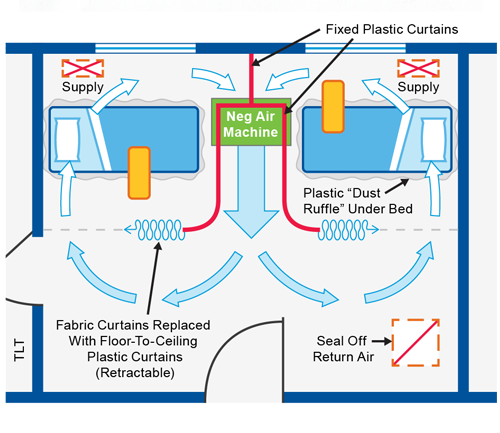
See How-To Document for guidance on creating or managing existing 2-resident or patient room.
- Expedient Patient Isolation Rooms How To
- Consider fire sprinkler coverage considering isolation curtains
- Inner resident and patient zones should not include recirculating HVAC wall units or HVAC return air grilles unless they can be sealed tight.
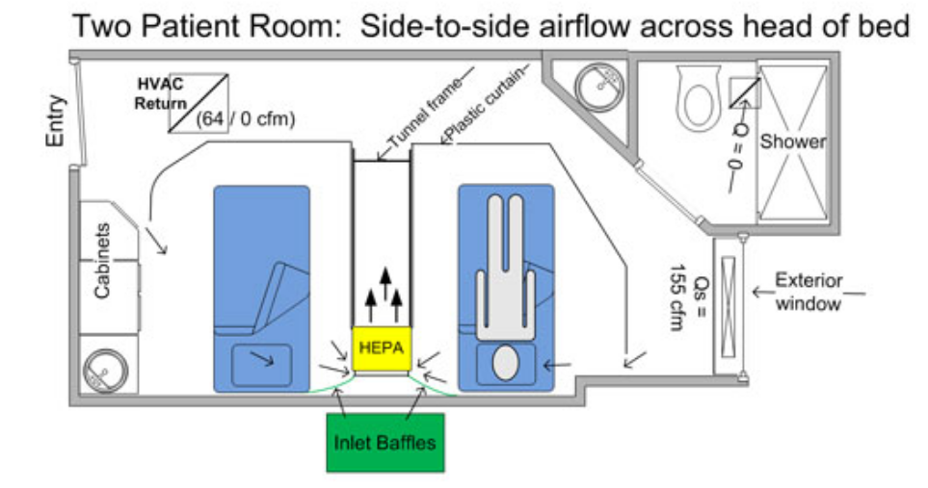
Consider Local Exhaust Source Control at Resident/Patient Head for Residents/Patients on CPAP, Nebulizer, or other AGP.

Resident/Patient Tent w HEPA (ie Demistifier)

Portable Snorkel Exhaust (ex. units used for soldering)
Ventilated Headboard (can be custom built on site)
Improve/Consider room airflow direction/patterns.
Look at Ventilated Headboards to capture resident/patient-generated aerosols closer to the source. New video from CDC/NIOSH of construction and research validation of ventilated headboard.
- Removal of Airborne Contamination in Airborne Infectious Isolation Rooms.
- Airflow Path Matters: Patient Room HVAC. ASHRAE Journal, vol. 58, no. 6, June 2016.
- CFD Analysis of Hospital Operating Room Ventilation System Part I: Analysis of Air Change Rates. ASHRAE Journal Vol. 60, no. 5, May 2018
- CFD Analysis of Hospital Operating Room Ventilation System Part II: Analyses of HVAC Configurations. ASHRAE Journal, Vol. 60, no. 6, June 2018
- Analysis of Spread Index: A Measure of Laboratory Ventilation Effectiveness. ASHRAE Conference Paper for the ASHRAE Annual Conference, Houston, TX. 2018
Transmission Through Air in Toilet Rooms | Return to Top
Studies have shown that toilets can be a risk of generating droplets and droplet residues from plumes in the air that could contribute to transmission of pathogens.
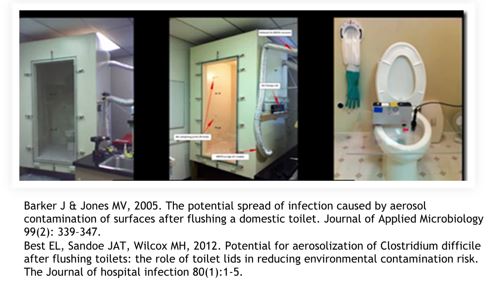
- Keep toilet room doors closed, even when not in use
- Put the toilet seat lid down, if there is one, before flushing
December 2018 – American Journal of Infection Control.
- C-Diff seeded in a toilet
- Water samples, settle plates, and air samples
- Spores present after 24 flushes
- Droplet nuclei spore bioaerosol produced over at least 12 flushes
Consider Maintaining 40-60% RH | Return to Top
Optimal relative humidity continues to be an area of active research.
Facilities/Maintenance – PPE | Return to Top
PPE Basics
- Refer to CDC Guidance on PPE use, especially banners at bottom of webpage.
- N95 masks require fit testing and a competent pulmonary efficiency.
- N95 masks are tested with 0.3 micron particles.
- certified to filter at least 95% of airborne particles.
- N95 masks are an effective tool for worker protection.
- Don’t forget vinyl gloves, goggles/eye protection, shoe covers, and disposable coveralls or bunny suits.
- After maintenance activities, wash hands with soap and water or use an alcohol-based hand sanitizer. Change clothes if soiled.
- Consider Re-Use : Silicone Half Mask with N95
- Double Glove Increases Protection When Re-Using Gear
HVAC System Maintenance and Filter Replacement During the Pandemic | Return to Top
- For HVAC systems suspected to be contaminated with SARS-CoV-2, it is not necessary to suspend HVAC system maintenance, including filter changes, but additional safety precautions are warranted.
- The risks associated with handling filters contaminated with coronaviruses in ventilation systems under field-use conditions have not been evaluated.
- Workers performing maintenance and/or replacing filters on any ventilation system with the potential for viral contamination should wear appropriate personal protective equipment (PPE):
- A properly-fitted respirator (N95 or higher)
- Eye protection (safety glasses, goggles, or face shield)
- Disposable gloves
- Consider letting the filter load up further than usual to reduce frequency of filter changes.
- Don’t let pressure drop increase enough to disrupt room pressure differentials.
- Confirm filters remain snug in their frames.
- When feasible, filters can be disinfected by lightly spraying with a 10% bleach solution or another appropriate disinfectant, approved for use against SARS-CoV-2, before removal. Filters (optionally disinfected or not) can be bagged and disposed of in regular trash.
- When maintenance tasks are completed, maintenance personnel should immediately wash their hands with soap and water or use an alcohol-based hand sanitizer.
Filter Changing in units serving COVID-19 residents/patients | Return to Top
- Consider letting the filter load up further than usual to reduce frequency of filter changes.
- Don’t let pressure drop increase enough to disrupt room pressure differentials.
- Confirm filters remain snug in their frames.
- Follow PPE Basics.
- Turn off AHU if possible. If not possible, consider wearing a bunny suit as additional PPE.
- Virus life on a filter is a function of temperature and relative humidity. Many folks utilize a fixative on the filters before they remove them. Spray with Lysol to disinfect and then use something like hairspray (spray paint works almost as well) to fixate.
- Bag the filter. It’s OK to throw out in regular garbage.
- Guidance for Filtration and Air-Cleaning Systems to Protect Building Environments from Airborne Chemical, Biological, or Radiological Attacks
Facilities / Maintenance | Return to Top
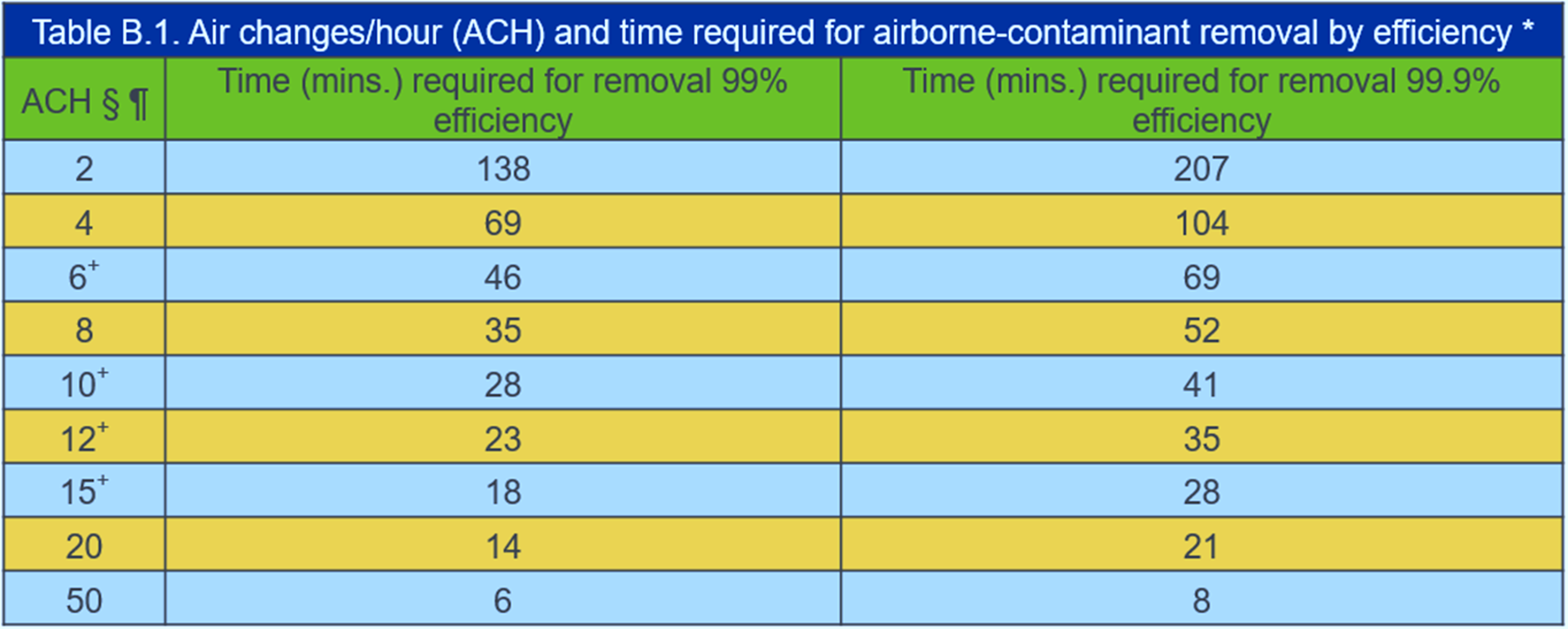
- Ventilate the Room and Terminal Clean before Re-use
- Follow CDC Air Change Clearance Rates (note these assume perfect mixing):
New Facility Design Considerations | Return to Top
- Provide HVAC systems with greater flexibility
- Consider centralized systems in lieu of room recirculation units
- Room recirculation units with better filtration capability
- Ability to increase outdoor air delivery
- Offer better room pressure control capabilities
- Floor Plans that improve environmental controls
- Isolation of wings for communities
- Isolation of wings for cohorted residents
- Permit creation of negative pressure areas
- Staff respite areas
- Staff or visitor screening areas
Residential Health Team Members | Return to Top
Below are the members of the Residential Health Team of the Epidemic Task Force
Jeremy Fauber HEAPY
Traci Hanegan Coffman Engineers, Inc.
Melvin Glass EMC Engineers
Jerry Ivey Willis-Knighton Health System
Mike Meteyer Erdman
Frank Mills Frank Mills Consulting
Jane Rohde JSR Associates, Inc.
Below are the members of the Healthcare Team of the Epidemic Task Force from which some of the information in this document was provided.
Traci Hanegan (Chair) Coffman Engineers, Inc.
Robert Block Dr. Robert M. Block, DDS
Mike Cummiskey Virginia Dept. of Health/Dental Division
Tim Earhart McDonough Bolyard Peck
David Eldridge Grumman/Butkus Associates
Jeremy Fauber HEAPY
Jonathan Flannery ASHE
Melvin Glass EMC Engineers
Eric Granzow Specialized Engineering Solutions
Rick Hermans Retired
Jerry Ivey Willis-Knighton Health System
Roger Lautz Affiliated Engineers Inc.
Mike Meteyer Erdman
Frank Mills Frank Mills Consulting
Zaccary Poots Toro-Aire Inc
Michael Sheerin TLC Engineering Solutions
Wayne Stoppelmoor Schneider Electric
Paul Supan American Dental Association Volunteer
Steven Welty Green Clean Air
Laurence Wilson WSP
Thanks to the following people who, along with members of the Healthcare Team, provided input, information, and review of the materials in the development of documents.
| Jane Rohde |
JSR Associates, Inc. |
| Kara Brooks |
ASHE |
| Mark Costello |
TLC Engineering Solutions |
| Bob Danner |
TLC Engineering Solutions |
| Jim Ferris |
TLC Engineering Solutions |
| Aaron Johnson |
TLC Engineering Solutions |
| Nicole Johnson |
Coffman Engineers, Inc. |
| Christoph Lohr |
ASPE |
| Ken Mead |
ASHRAE TC9.6 Healthcare Facilities |
| Luca Piterà |
AICARR |
| Ben Roseborough |
TLC Engineering Solutions |
| Kevin Scarlett |
Washington State Department of Health |
| Jeff Stone |
TLC Engineering Solutions |
| John Williams |
Washington State Department of Health |